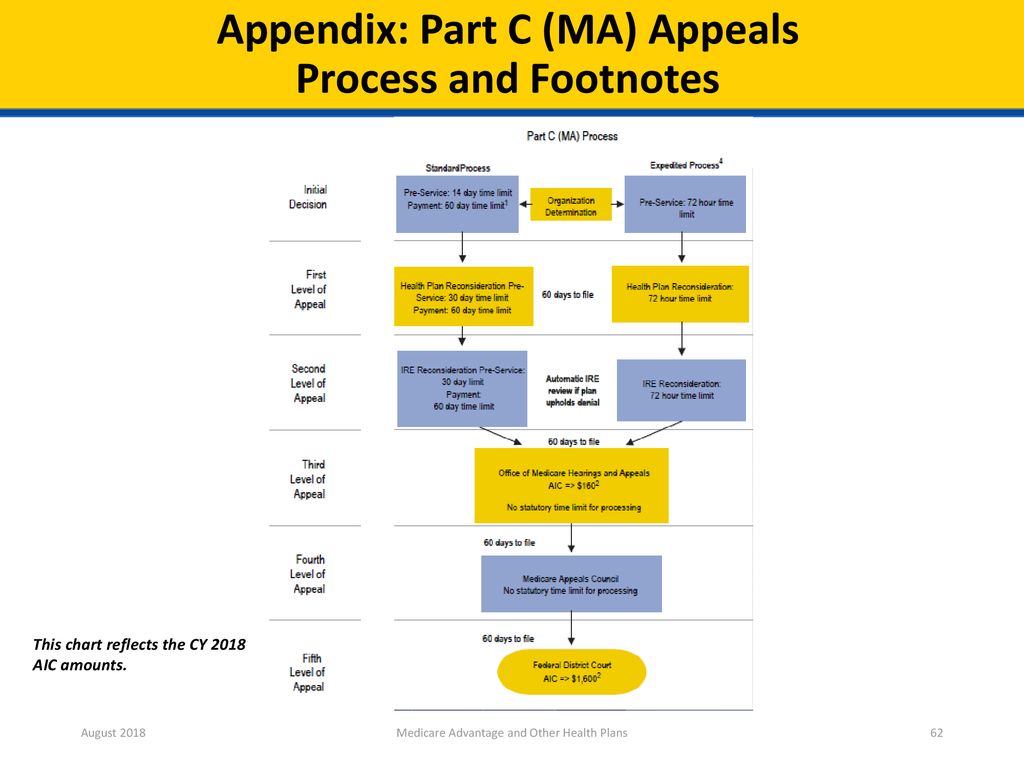
38 medicare appeals process diagram
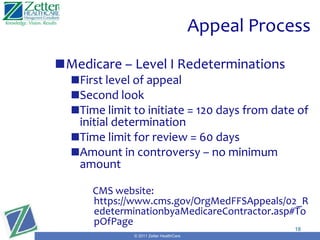
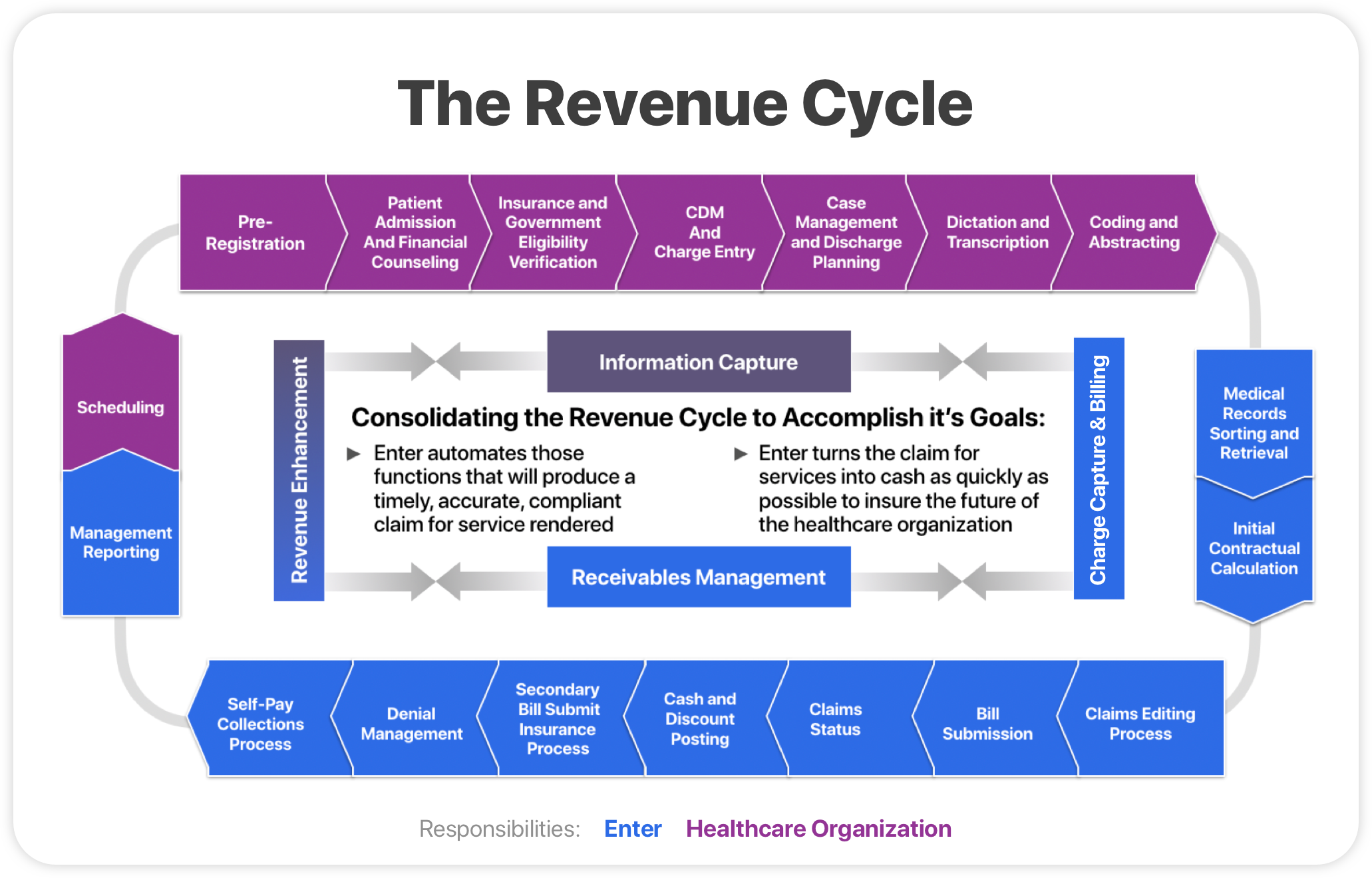
PDF Pharmacy Billing and Reimbursement Medicare Appeals Process: There are 5 steps after an initial denial (coverage determination)from the insurance company that may take place to substantiate a patients or providers request for a particular non covered medication. 1. Level 1: Redetermination from plan (Appeal)-can be for any denied coverage Flow chart of medical billing It's at this stage that a claim may be accepted, denied, or rejected. Effectively, a claims appeal is the process by which a provider attempts to secure the proper reimbursement for their services. This can be a long and arduous process, which is why it's imperative that billers create accurate, "clean" claims on the first go. Patient Statement :
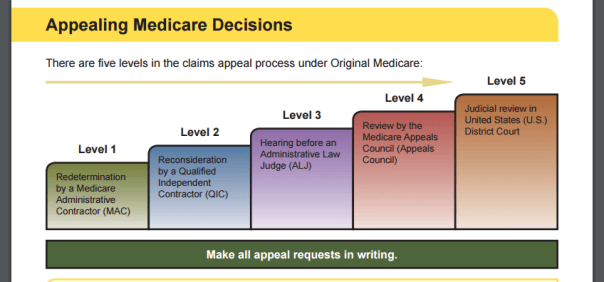
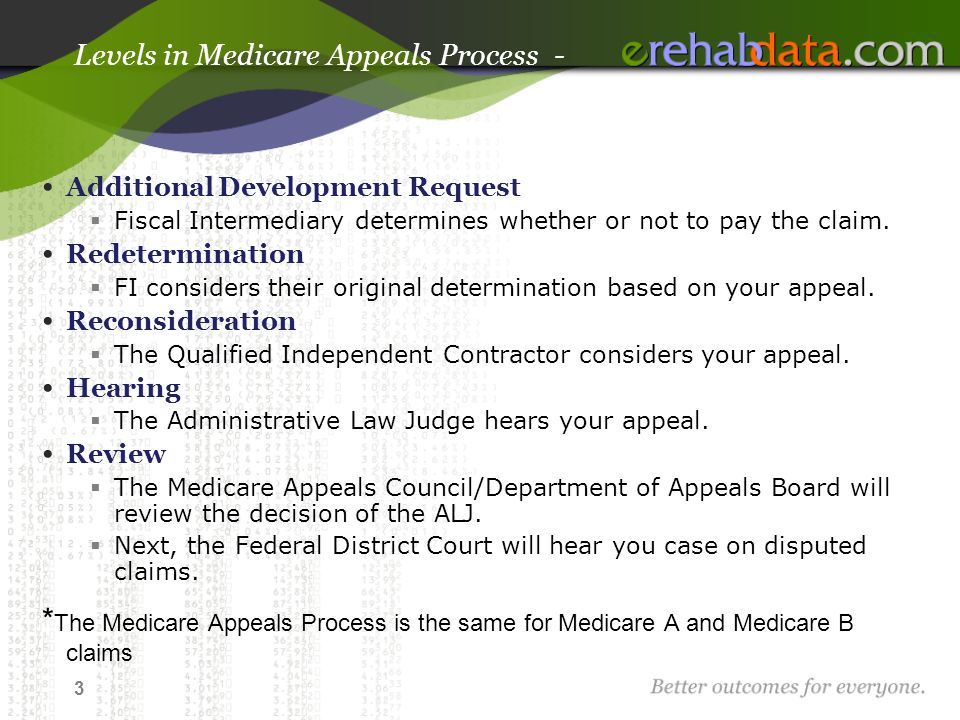
Medicare appeals process diagram" Keyword Found Websites ... Medicare offers five levels in the Part A and Part B appeals process The levels, listed in order, are: • Redetermination by an FI, carrier or MAC • Reconsideration by a QIC • Hearing by an Administrative Law Judge (ALJ) • Review by the Medicare Appeals Council within the Understanding the Medicare Appeal Process Medicare

Medicare appeals process diagram
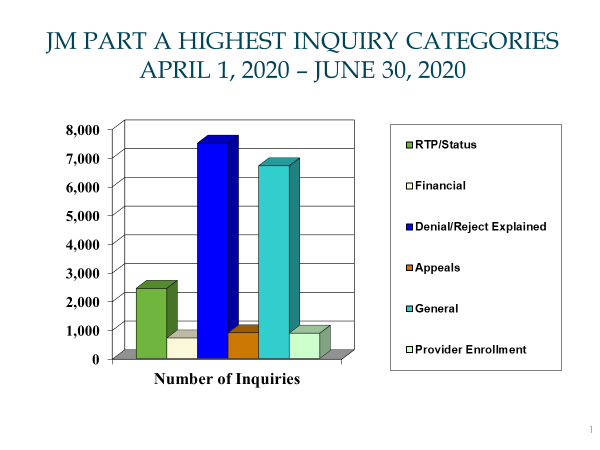
Medical Insurance Chapter 13 Flashcards - Quizlet How many steps are there in the Medicare appeals process? 5. What are the five steps in the Medicare appeals process? 1. Re determination 2. Reconsideration 3. Administrative Law Judge 4. Medicare Appeals Council ... Diagrams. Flashcards. Mobile. Help. Sign up. Help Center. Honor Code. Community Guidelines. Teachers. About. Company. Blog. Press ... Getting to the root causes of denials - hfma A review of denial and audit data can help providers prevent errors that lead to denials, and in the process reduce financial loss and increase resource efficiency. 3 emerging trends call for a proactive denial and appeal strategy. A proactive approach is essential to identifying root causes as the basis for denial management and prevention. Trace Help - Vyne Medical Electronically submit medicare appeals and discussion requests for more timely submission and reimbursement. Overview. Simplify the process of receiving and responding to audit requests from the Centers for Medicare & Medicaid Services (CMS) with the Refyne platform.
Medicare appeals process diagram. PDF Alabama Medicaid Agency Policy and Procedure Manual program, Medicare. Medicare is a health insurance program primarily for elderly persons, regardless of income. It is financed through Social Security taxes and premiums. Medicaid is jointly financed by the state and federal governments and is designed to provide health care to low income individuals. Medicaid started in PDF Your Guide To The Disability Process Chapter 3 - Health Insurance Issues Before and After Medicare This chapter explains Medicare and Medicaid eligibility issues disabled patients often have. It also contains guidance for disabled patients enrolled in group health insurance programs. Chapter 4 - Appeals Process This chapter addresses the process through which you can file an ... appeal or grievance on Health - Medical Insurance How to file Appeals & Grievances PO Box 629007 El Dorado Hills , CA 95762 - 9007 Fax: (916) 350 - 7585. CA Department of Insurance. IMR - Independent Medical Review. REQUEST FOR REVIEW Molina Health Care OF CANCELLATION, RECISSION, OR NONRENEWAL OF HEALTH CARE SERVICE PLAN BENEFITS. hhs.gov/curbing-insurance-cancellations. PDF Palmetto GBA: The Review Choice Demonstration (RCD) for ... Medicare Trust Funds from improper payments, and the reduction of Medicare appeals • CMS expects that creating a review choice process will ensure that Medicare coverage and documentation requirements are likely met August 2019 Review Choice Demonstration (RCD) • RCD does not create new documentation requirements
Filing Medicare Advantage Plan appeal| Medicare Start the process: Follow the directions in your plan's initial denial notice and plan materials. You have 60 days from the date of the coverage determination. If you miss the deadline, you must provide a reason for filing late. See what information to include in your written request. beautyathomeshop.de › sc-dew-my-benefits-loginSc dew my benefits login - beautyathomeshop.de Columbia, SC 29202. Employ scuihub. org has ranked N/A in N/A and 149,288 on the world. NY. Find it by Audience Workers. Contacts for Unemployment: Toll-Free: 1-800-593-7660 (Customer services available Mon-Fri, Dec 18, 2021 · my benefits portaluse case diagram for online furniture shopping. 1724). Transaction History. - Main - MSP Recovery one of the largest spac combined company to be listed on nasdaq learn more transactions announced: $32.6 billion the u.s. healthcare system learn more msp recovery and palantir partner to transform connectivity across claims recoveries to virage capital management learn more msp recovery enters into $3 billion agreement to sell select healthcare in federal appeal learn more doj supports msp ... › regulations › formsForm 8584, Nursing Comprehensive Assessment | Texas Health ... Form 8584 is an assessment that contains all of the required elements of a comprehensive nursing assessment. The program provider may choose to create their own tool, provided it has all of the required elements. Form 8584 is used by registered nurses (RNs) in Home and Community-based Services (HCS ...
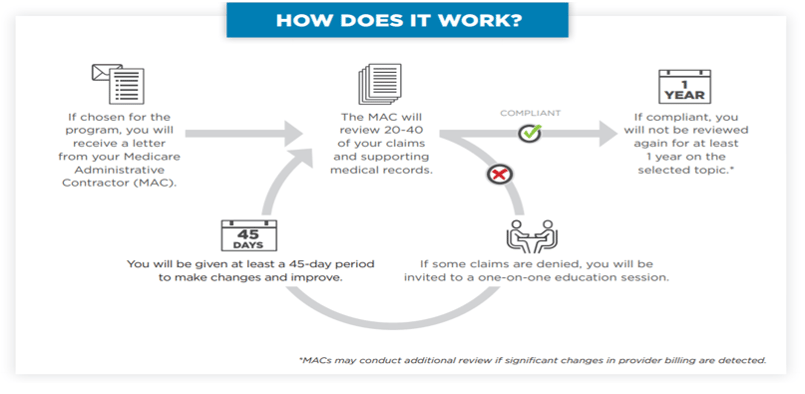
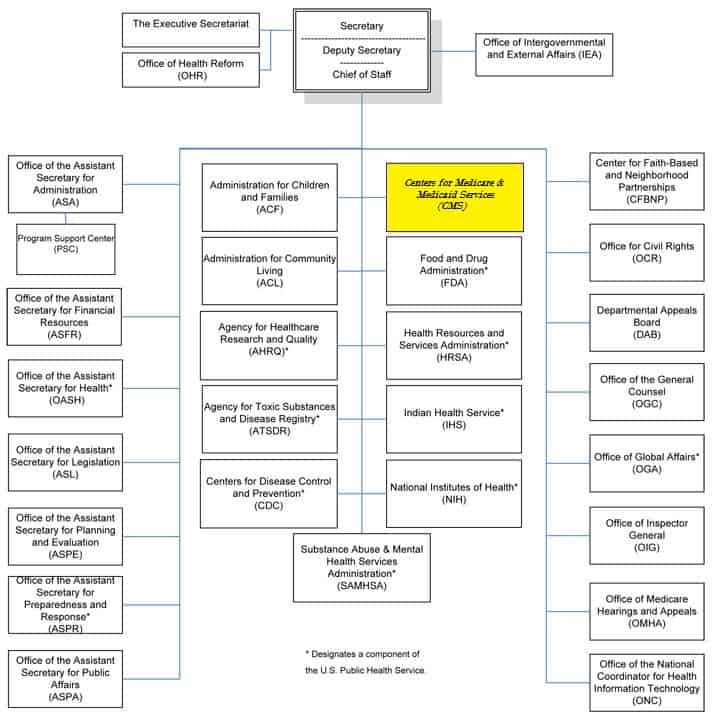
› Medicare › Medicare-ContractingWhat's a MAC | CMS - Centers for Medicare & Medicaid Services Jan 12, 2022 · A Medicare Administrative Contractor (MAC) is a private health care insurer that has been awarded a geographic jurisdiction to process Medicare Part A and Part B (A/B) medical claims or Durable Medical Equipment (DME) claims for Medicare Fee-For-Service (FFS) beneficiaries. Part A Novitasphere User Manual - Novitas Solutions • Medicare Beneficiary Demographics • Date of Death • Unlawful Occurrences • Medicare Part B Entitlement • MDPP Coverage • ESRD - Medicare Beneficiaries in an active ESRD occurrence are not MDPP eligible. • Medicare Advantage (MA) Enrollment(s) - Contact the MA plan for MDPP Coverage Information. PDF Medicare Recovery Audit Contractors (RACs): An Overview RAC Program's Three Keys to Success 1. Minimize Provider Burden 2. Ensure Accuracy 3. Maximize Transparency 6 6 Minimize Provider Burden Limit the RAC "look-back period" to three years yMaximum look back date is October 7, 2007 RACs will accept imaged medical records on CD/DVD Example of a Grievance Procedure that Incorporates Due Process Procedure: Grievances must be submitted to the Section 1557 Coordinator within (60 days) of the date the person filing the grievance becomes aware of the alleged discriminatory action. A complaint must be in writing, containing the name and address of the person filing it.
How do I file an appeal? | Medicare The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal. note: Write your Medicare Number on all documents you submit with your appeal request.
› Medicare › Appeals-and-GrievancesOriginal Medicare (Fee-for-service) Appeals | CMS May 07, 2020 · To see a diagram (flowchart) of the original Medicare (fee-for-service) standard and expedited appeals process, go to the "Downloads" section below. Appointment of Representative. A party may appoint any individual, including an attorney, to act as his or her representative during the processing of a claim(s) and /or any claim appeals.
PDF Healthcare Transactions & Medicare's Change of Ownership ... • Use "before and after" diagrams in dealing with regulators • If a sub-unit has its own Medicare agreement, then you must submit a separate 855 • Distinguish between changing provider types (requires initial enrollment) and provider sub-types (can be part of a CHOW) • Tax Identification Numbers should not always control the
Flow Chart: Appeals Process & Levels. Source: Centers for ... Download scientific diagram | Flow Chart: Appeals Process & Levels. Source: Centers for Medicare & Medicaid Services from publication: UNDERSTANDING & RESPONDING TO PREPAYMENT REVIEWS FOR ...
Chapter 16 Medical insurance Flashcards - Quizlet The third level of Medicare appeals a health care provider may use if they disagree with a claims reconsideration decision. The hearing provides an opportunity to explain your position to an administrative law judge. A listing of outstanding accounts that have not been paid.
The 5 Levels of the Appeals Process - CGS Medicare The 5 Levels of the Appeals Process There are 5 levels of appeals available to you: Redetermination Reconsideration Administrative Law Judge (ALJ) Departmental Appeals Board (DAB) Review Federal Court (Judicial) Review Level 1 is a Redetermination, which is conducted by the DME MAC.
Medicare Managed Care Appeals & Grievances | CMS Medicare health plans, which include Medicare Advantage (MA) plans - such as Health Maintenance Organizations, Preferred Provider Organizations, Medical Savings Account plans and Private Fee-For-Service plans - Cost Plans and Health Care Prepayment Plans, must meet the requirements for grievance and appeals processing under Subpart M of the Medicare Advantage regulations.
Appeals and Grievances Process | UnitedHealthcare ... Send the letter or the Redetermination Request Form to the Medicare Part C and Part D Appeals and Grievance Department PO Box 6103, MS CA124-0197, Cypress CA 90630-0023.You may also fax your letter of appeal to the Medicare Part D Appeals and Grievances Department toll-free at 1-877-960-8235 or call 1-877-614-0623 TTY 711. 8.a.m. - 8 p.m.: 7 ...
Apache Server at Port 80
Medicare Advantage Appeals & Grievances | UnitedHealthcare Medicare Advantage Plans The following procedures for appeals and grievances must be followed by your Medicare Advantage health plan in identifying, tracking, resolving and reporting all activity related to an appeal or grievance. Coverage decisions and appeals Asking for coverage decisions Where to submit a request for a coverage decision
Level 1 Appeals: Medicare Advantage (Part C) - HHS.gov Level 1 Appeals: Medicare Advantage (Part C) If you are in a Medicare Advantage plan, you can appeal the plan's decision to not pay for, not allow, or stop a service that you think should be covered or provided. You may contact your plan or consult your plan materials for detailed information about requesting an appeal and your appeal rights.
PDF Training - Medicare complaints including appeals ... 1. Complaints Process, two-page document 2. Medicare Appeals, 60 -page booklet 3. Making Sense of Your Medicare Statements, three-page document 4. Medicare redetermination reque st form — 1st Level of appeal, one- page document 5. Welcome to Livanta, the BFCC-QIO for Washington, one- page document 6.
MITA Business Process Areas (Categories) and Processes ME08 Manage Member Grievance and Appeal (Under Development) ME03 Perform Population and Member Outreach (Under Development) Operations Management (OM) Payment and Reporting OM14 Generate Remittance Advice OM18 Inquire Payment Status OM27 Prepare Provider Payment OM28 Extract Information Claims Adjudication OM07 Process Claims
Medicare Advantage Appeals Process - NappingCat Health The Medicare Advantage appeals process includes four levels of review by several entities. At each level of review, a denied claim may be overturned, partially overturned, or upheld. The Center for Medicare and Medicaid Services (CMS) refers to the insurance company and the Medicare Advantage plans they promote as Medicare Advantage ...
› resources › templatesInvestigation Templates & Downloads For Successful ... - i-Sight Templates are designed to make your job easier, by providing a framework you can use to complete reports, forms and other formatted documents used in the investigations process. i-Sight’s templates are free, downloadable and editable, ensuring their usefulness for a wide variety of systems and processes.
Trace Help - Vyne Medical Electronically submit medicare appeals and discussion requests for more timely submission and reimbursement. Overview. Simplify the process of receiving and responding to audit requests from the Centers for Medicare & Medicaid Services (CMS) with the Refyne platform.
Getting to the root causes of denials - hfma A review of denial and audit data can help providers prevent errors that lead to denials, and in the process reduce financial loss and increase resource efficiency. 3 emerging trends call for a proactive denial and appeal strategy. A proactive approach is essential to identifying root causes as the basis for denial management and prevention.
Medical Insurance Chapter 13 Flashcards - Quizlet How many steps are there in the Medicare appeals process? 5. What are the five steps in the Medicare appeals process? 1. Re determination 2. Reconsideration 3. Administrative Law Judge 4. Medicare Appeals Council ... Diagrams. Flashcards. Mobile. Help. Sign up. Help Center. Honor Code. Community Guidelines. Teachers. About. Company. Blog. Press ...




.png)







0 Response to "38 medicare appeals process diagram"
Post a Comment